Advocacy

Want to Support HFM?
Want to join our efforts but not sure where to start? Make a donation, join our Foundation as a member or volunteer your time and take advantage of this incredible opportunity to lend your support. These are great ways to contribute to our causes, and every little bit goes towards supporting the mission of the Hemophilia Foundation of Maryland.
Advocacy
Help is Our Main Goal
We influence those who make a difference
 We have a stated mission to advocate on behalf of our members. Advocacy happens every day and there are many ways to participate in advocacy activities throughout the year, including:
We have a stated mission to advocate on behalf of our members. Advocacy happens every day and there are many ways to participate in advocacy activities throughout the year, including:
- Writing letters to your elected officials regarding proposed changes to law or regulations
- Meeting with other state decision-makers, including state departments of insurance and Medicaid agencies
- Educating health plans about the needs of the bleeding disorders community
- Educating schools and employers about the needs of the bleeding disorders community
- Advocating to your health care provider about your unique health care needs
If you are interested in learning more about advocacy and becoming a better advocate, take a few moments to explore the tools and resources below:
Maryland State Resources
- Hemophilia Federation of America - VISIT WEBSITE
- National Hemophilia Foundation - VISIT WEBSITE
- House of Representatives - VISIT WEBSITE
- U.S. Senate - VISIT WEBSITE
- U.S. Congress - VISIT WEBSITE
- Centers for Disease Control and Prevention - VISIT WEBSITE
- The Food and Drug Administration - VISIT WEBSITE
Copay Accumulator Patient Impact:
In the age of high deductibles and patient out of pocket expenditures, more and more people depend on copay assistance to afford their life-saving specialty medications. This video demonstrates how Copay accumulator adjustments affect patients requiring specialty medications with no generic alternatives. Learn more at hemophilia.org
Hemophilia Foundation of Maryland (HFM)
13 Class Court Parkville, MD 21234

07/23/2024 – Press Release – Comer Releases Report on PBMs’ Harmful Pricing Tactics and Role in Rising Health Care Costs
WASHINGTON—Today, House Committee on Oversight and Accountability Chairman James Comer (R-Ky.) issued a report outlining how the three largest Pharmacy Benefit Managers (PBMs) —CVS Caremark, Express Scripts, and OptumRx—have monopolized the pharmaceutical marketplace by deploying deliberate, anticompetitive pricing tactics that are raising prescription drug prices, undermining community pharmacies, and harming patients across the United States. The House Oversight Committee will hold a hearing with PBM executives today at 10:00am ET.
“Instead of prioritizing the health of Americans across the country, evidence obtained by the House Oversight Committee shows how the three largest pharmacy benefit managers colluded to line their own pockets. These self-benefitting pricing tactics pushed by PBMs have done nothing but jeopardize patient care, undermine local pharmacies, and raise prescription drug prices,” said Chairman Comer. “Since 2021, the Committee has made it a priority to expose harmful PBM practices and advance legislative solutions to ensure greater transparency and accountability in the PBM industry. Americans deserve access to affordable, life-saving medications and the Committee will continue to work in a bipartisan fashion to shine a light on PBMs and restore competition in the pharmaceutical marketplace.”
Today’s report, entitled “The Role of Pharmacy Benefit Managers in Prescription Drug Markets,” includes evidence obtained by the Committee showing how PBMs inflate prescription drug costs and interfere with patient care for their own financial benefit. The report concludes that the present role of PBMs in prescription drug markets is failing and requires Congress and states to implement legislative reforms to increase the transparency of the PBM market.
Below are key findings from the report:
The three largest PBMs have used their position as middlemen and integration with health insurers, pharmacies, providers, and recently manufacturers, to enact anticompetitive policies and protect their bottom line. The Committee found evidence that PBMs share patient information and data across their many integrated companies for the specific and anticompetitive purpose of steering patients to pharmacies a PBM owns. Furthermore, the Committee found that PBMs have sought to use their position to artificially reduce reimbursement rates for competing pharmacies.
PBMs frequently tout the savings they provide for payers and patients through negotiation, drug utilization programs, and spread pricing, even though evidence indicates that these schemes often increase costs for patients and payers. The Committee identified numerous instances where the federal government, states, and private payers have found PBMs to have utilized opaque pricing and utilization schemes to overcharge plans and payers by hundreds of millions of dollars.
The largest PBMs force drug manufacturers to pay rebates in exchange for the manufacturers’ drugs to be placed in a favorable tier on a PBM’s formulary, making it difficult for competing, lower-priced prescriptions (often generics or biosimilars) to get on formularies. The Committee has found evidence that PBMs regularly place higher cost medications in more preferable positions based on their formularies, even when there are lower-cost and equally safe and effective competing options.
As many states and the federal government weigh and implement PBM reforms, the three largest PBMs have begun creating foreign corporate entities and moving certain operations abroad to avoid transparency and proposed reforms. The Committee found that these PBMs have created group purchasing organizations (GPOs) to centralize the negotiation of rebates and fees in Switzerland and Ireland. They have also created companies in Ireland and the Cayman Islands to manufacture and market certain highly profitable generics and biosimilars. The creation of entities in locations well known for their lack of financial transparency and movement of operations that would be subject to impending regulations only heightens concerns that PBMs will do anything to avoid transparency.
The largest PBMs’ use of tools such as prior authorizations, fail first policies, and formulary manipulations have significant detrimental impacts on Americans’ health outcomes. The Committee found that the use of these tools enables PBMs to slow the market uptake of cheaper generics and biosimilars. Furthermore, the Committee found that these tools often delay and negatively impact patient care. Read More
Upcoming CareFirst Formulary Updates and Medications Added to Prior Authorization List
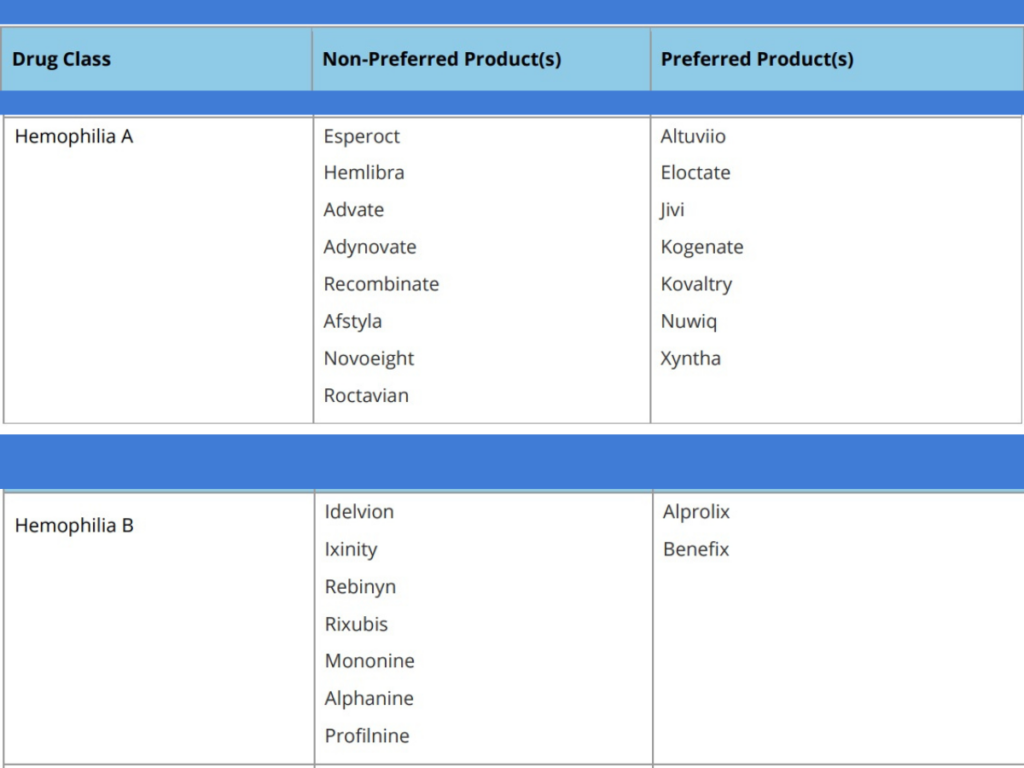
Carefirst has issued a Medical Preferred Drug Strategy Update effective August 1, 2024. Below is a summary of the factor agents affected.
What this means for affected patients:
- If a patient is taking a non-preferred medication, they can continue to take that medication until the current prior authorization expires.
- If a patient needs to continue medication therapy with the non-preferred medication, their doctor can submit a new prior authorization upon the expiration date of the current prior authorization.
- The new prior authorization may result in an approval for an alternative, preferred medication, which is as clinically effective and safe as the non-preferred medication.
- If their doctor believes the non-preferred medication must be continued, their doctor can submit information within the new prior authorization request to obtain a medical necessity exception.

New Federal Rule Strengthening Protections Against Disability Discrimination
May 14, 2024 – By BD SUMHAC, HFA, and NBDF
Progress Alert! After advocacy from the bleeding disorders community, the U.S. Department of Health and Human Services (HHS), through its Office for Civil Rights (OCR), finalized a new rule that increases equity and access to behavioral health facilities for people with bleeding disorders.
The new rule, entitled Discrimination on the Basis of Disability in Health and Human Service Programs or Activities, clarifies that the protections afforded to people with disabilities (including people with bleeding disorders) under Section 504 of the Rehabilitation Act of 1973 (Section 504) apply to medical settings.

HFM Advocacy: Accumulator Adjustment Programs
Make all Copays Count!
Many bleeding disorder patients use co-pay assistance, such as co-pay cards or manufacturer coupons, to pay for their life-saving medications. Pharmacy benefit managers (PBMs) and insurers increasingly use co-pay accumulator programs to prevent such assistance from counting towards patient cost-sharing, such as their deductible or annual out-of-pocket maximum. As a result, patients may struggle to afford and adhere to their medications as insurers and PBMs seek to shift more cost-sharing responsibilities to patients.
The Issue
Accumulator adjustment programs prevent any co-payment assistance that may be available for high-cost specialty drugs from counting toward a patient’s deductible or maximum out-of-pocket expenses.
Many pharmaceutical manufacturers offer co-pay cards that help cover a patient’s portion of drug costs. Traditionally, pharmacy benefit managers have allowed these co-pay card payments to count toward the deductible required by a patient’s health insurance plan. With an accumulator adjustment program, patients are still allowed to apply the co-pay card benefits to pay for their medications up to the full limit of the cards, but when that limit is met, the patient is required to pay their full deductible before cost-sharing protections kick in.
Patients are often unaware they are enrolled in one of these programs until they go to the pharmacy counter and realize they must pay the full cost of their medication, leading them to abandon or delay their prescription. These programs can be called different names, are often marketed as a positive benefit, and are usually disclosed many pages into plan materials, leading to a lack of awareness about them to patients.
Example: It’s the start of a new health plan year in January, and you are on a biologic with a list price of $3,000 a month. You use your co-pay card at your specialty pharmacy and make a regular co-payment. By the time March arrives, you’ve reached the limit on your co-pay assistance. As a result, when you refill your prescription in April, you will owe $3,000, the full cost of your drug, because the deductible has not yet been paid down.
The Solution
When calculating a patient’s overall contribution to any out-of-pocket maximum or any cost-sharing requirement, a health plan must include any amounts paid by the patient or paid on behalf of the patient by another person.
The Trends
People most likely to be enrolled in co-pay accumulator adjustment programs include those with employer-sponsored insurance plans, particularly individuals enrolled in high-deductible health plans (HDHPs). HDHPs have become increasingly popular as employers and insurers seek opportunities to incentivize appropriate health care utilization and to lower costs.
*Source: American Journal of Managed Care, Impact of a Co-pay Accumulator Adjustment Program on Specialty Drug Adherence
Our Work
The All Co-pays Count Coalition (ACCC) was formed to collaborate amongst the patient and provider community around legislative and patient education efforts on a federal and state level. Hemophilia Foundation of Maryland is a member of the ACCC.
We are looking for community members who have been impacted by a Copay Accumulator Adjustment Program. Please email HFM.


